I’m overwhelmed. Odds seemed to be stacking against me. I was devastated.
I did well with surgery. It went fairly smoothly and I would call it a success. But remember that to get this surgery, I made the mistake, perhaps, of taking a break from treatment. The reason I say it may have been a mistake is because of the last three days.
I was feeling better. I am eating well. But a few days ago, I began to swell in my belly for no reason. There are other gross symptoms as well. After a truly miserable night, I saw the PA oncologist. She felt that the swelling is something called ascites — a buildup of fluid in the abdomen that happens as your liver begins to fail. But she also confirmed that my liver is enlarged. And the bloodwork that no one took throughout my surgery showed the truth: all the numbers look quite dismal.
The hernia surgeon — a really great surgeon who is highly empathetic — had seen the “tumors” as he moved though my abdomen. That idea alone sat poorly with me. But then I developed these symptoms.
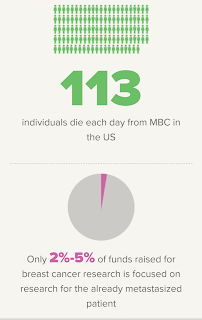
The situation is so complicated. Apparently, Eribulen requires good liver function, which I do not have any longer. So it is off the table. Another chemo may do, or the PA mentioned something I immediately zeroed in on: my doctor might feel there are no more options.
I am not ready. I want any option. I want to make it through the holidays. I want to turn the train around and become one of those miracle sisters I hear from in my Facebook Mets groups.
So today, I went to get the fluid drained. They couldn't find enough to drain.
No ascites.
Then I heard from the providers. I will start the different chemo -- Doxil -- tomorrow.
Yesterday, maybe I had weeks. Today,. possibilities again present themselves.
This disease is maddenimg.
I am headed for more rough times. Painful mouth sores, hand and foot syndrome, GI issues. But I'm ready for that. I not ready to die.
I thought I would be gracious when I faced death but it has come up on me so suddenly...I just can’t process.
Your prayers, positive energy, good thoughts and love — all welcome. Just as I am no hero with pain and physical difficulty, it turns out I am just as bad at dying. I am certainly raging against the dying of the light, as Dylan Thomas suggested.
Do not go gentle into that good night
Do not go gentle into that good night,
Old age should burn and rave at close of day;
Rage, rage against the dying of the light.
Though wise men at their end know dark is right,
Because their words had forked no lightning they
Do not go gentle into that good night.
Good men, the last wave by, crying how bright
Their frail deeds might have danced in a green bay,
Rage, rage against the dying of the light.
Wild men who caught and sang the sun in flight,
And learn, too late, they grieved it on its way,
Do not go gentle into that good night.
Grave men, near death, who see with blinding sight
Blind eyes could blaze like meteors and be gay,
Rage, rage against the dying of the light.
And you, my father, there on the sad height,
Curse, bless, me now with your fierce tears, I pray.
Do not go gentle into that good night.
Rage, rage against the dying of the light