Surviving Pinktober
Here we are, some 30 days later. We survived Pinktober.
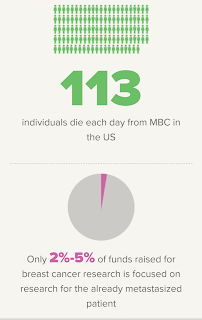
In terms of awareness for metastatic breast cancer, I think we are making strides. Susan G. Komen upped their ante, giving more for Metastatic Breast Cancer research. I saw multiple fundraisers for my favorites, like METAvivor and others. I feel like my mets sisters and I are making strides in making the point: you will never conquer cancer until you conquer metastatic cancers. Stage IV needs more.
And more happy news: I did not get one single “Check your boobies” or “Put a heart on your timeline” message the entire month. Ok, the last one was September 28, but still! Good job, everyone! Thanks for showing your love for me and the sisters.
My Update: No Reuptake!
So, my own update: in a twist I have barely adjusted to, I’m doing…well.
I know, right? No, I’m not cured, and I never will be. I’m not really even No Evidence of Disease (NED) or No Evidence of Active Disease (NEAD) for bones yet. But my PET scan showed some really amazing findings.
I’ve become adept at reading findings. I can speak the speak decently well. Yet, the radiologist who wrote these seems to write especially obtuse findings. All findings are obtuse to lay people, but this one seems to contain double…positives. For instance:
There is interim significant decrease to normalization of the previously demonstrated diffuse hyper metabolism throughout the axial and proximal appendicular osseous structures, correlated with heterogenous osteoblastic disease consistent with diffuse osseous metastases.
(The interpretation, as best I am able: the uptake to my bones is significantly decreased.)
She goes on:
There has been interval resolution of hyper metabolic soft tissue nodules along the anterior chest wall in comparison to prior PET/CT.
(Now this is really good, because I still feel areas of concern: my chest wall is resolved. Hooray for the radiation!)
And
The previously described hepatic lesions, best appreciated on the MRI dated January 22, 2018, are essentially inconspicuous relative to expected heterogeneity of background liver uptake.
(The lesions on my liver are disappearing and nearly gone compared to the last one.)
So the report boils down to this: a really good response, with some remaining mets to my bones. It’s like a miracle, except it’s medical science.
To be clear: I’m not fully NED or NEAD yet. I can still see them in my bones. I can still see a few spots on my liver — boy, was that liver much worse than I realized. I once again dodged a bullet. I may have more time than the statistics would suggest.
I’m not used to this. I’m not used to being the one who gets good news. I’m used to being the one who weeps at home with hubby and then puts a brave face on for others. Since I began the path of recurrence, I have received one load of bad news after another. I’d think I was cancer free, only to learn I was metastatic. I would think I was getting better, only to find another structure that was affected. I have been through moments where I thought body systems were shutting down; I’ve been through tremendous pain, malaise, nausea and GI, a flu like you’ve never felt before — and even the pain from adjusting to this medication, which I still have to take cautiously.
But dayum, it’s working! Thank God I didn’t quit as I thought I would.
To what do I owe this? Radiation gave me a boost, for sure. I’m taking the following: Lynparza 150s, twice a day (half the former dose), along with an over the counter drug called Pyridium to avoid that extra pain. I’m also taking a completely different formulation of my thyroid meds, with much more faster-acting T3 and much less T4 — a move which seems to have addressed that obstacle that I’ve written about: that the thyroid meds seem to encourage the cancer. I’m also taking a daily hemp-based CBD supplement when I’m in Michigan or wherever it’s legal.
And the other thing: I feel well. Not perfect; I still nap nearly every day. I can’t manage a long walk. I still have to juggle, um, GI and urinary discomfort. I can, however, enjoy life again. It's been so long, I had forgotten how it feels. And, the hardest part to adjust to, I can stand down a bit. I feel like I can stop waiting for the other shoe to fall.
So. Now What?
We in the community know that this good situation will eventually end. The cancer will overcome this defense. It could happen in a month, but the good news is that it could even be one, five or even 10 years. And they may not be 10 years of misery so much as impairment. And I will still have scans and pokes and big pills to swallow daily for the rest of whatever time I am permitted.
I can’t tell you how blessed and grateful I feel. Medical science is amazing. I've been given a gift.
Let me thank God and you all for your love and support. I wouldn't be here without it.